Tarsal Coalition
Background
CT scan showing a calcaneo-navicular coalition
The hindfoot normally consists of three “tarsal bones”: the talus (top bone), calcaneus (bottom/back bone), and navicular (front bone). These three bones have small joints between them, and those joints allow the side-to-side motion of your foot and ankle that is important for walking and athletic activity.
A “tarsal coalition” is an abnormal connection between two of these bones. When this occurs, the bones can’t move independently from each other, and the side-to-side motion of our ankle is limited. The foot and ankle become stiff, which inhibit adaptation to uneven surfaces or sudden changes in position. As a result, ankle sprains, fractures, arthritis, deformity, and pain become more common.
Tarsal coalitions are generally present at birth, and can be associated with other problems or occur on their own. Children with coalitions normally adapt pretty well, and the condition remains asymptomatic throughout youth. It is not until they are a little older—typically in their teens or twenties—that the coalitions start causing problems.
The most common presentation is an adolescent or young adult with recurrent ankle sprains and unexplained ankle pain.
Types of Tarsal Coalitions
There are two main areas in which tarsal coalitions occur: The first is on the lateral side (or outside) part of the foot, between the calcaneus and the navicular bones; these are called “calcaneo-navicular coalitions.” The second is on the medial side (or inside) part of the foot, between the talus and the calcaneus bones; these are called “subtalar coalitions.”
Diagnosis
At your first visit, Dr. Bohl will closely examine your foot and ankle. He will test for each of the normal motions between the bones of your hindfoot. He will examine for the deformities classically associated with coalitions. And he will palpate for the abnormal bony connections, which can sometimes be felt easily directly through the skin.
Dr. Bohl will then obtain x-rays of the foot and ankle. Some tarsal coalitions are obvious on simple x-rays. Others are not obvious, but have subtle signs suggestive of the abnormal connections. X-rays are also useful for identifying any associated arthritis or deformity, and for ruling out other problems that could be contributing to your symptoms.
Ultimately, if a tarsal coalition is suspected, the gold standard for diagnosis is CT and/or MRI. Dr. Bohl will order one or both of these images, which will allow 3D visualization and examination in multiple planes. He will generally then want to see you back in the office to review the images with you in person.
Nonsurgical Treatment
Physical therapy is an important part of nonsurgical management for tarsal coalition
Patients should initially attempt management of tarsal coalitions without surgery. Such treatment includes physical therapy, non-steroidal anti-inflammatory medications (either topical or oral), boot immobilization, ice, rest, and bracing. With these interventions and time, the coalition may become less symptomatic.
The first phase of treatment is focused on cooling down acute inflammation. If severe, Dr. Bohl will typically recommend wearing a CAM boot for a month or so.
The second phase of treatment is focused on rehabilitation and prevention of recurrent symptoms. For coalitions, this always involves physical therapy with a focus on ankle proprioception and strength.
Surgical Treatment
After attempted nonsurgical treatment, many patients will elect for surgical correction of this anatomic problem. There are several different surgical procedures, and the best choice depends on the location of the coalition, the size of the coalition, associated conditions such as arthritis or deformity, the patient’s age, and the activity level and goals of the patient.
The most common procedure that Dr. Bohl performs for tarsal coalitions is resection of a calcaneo-navicular coalition. In this procedure, a small 4cm incision is made over the top of the foot near the ankle. After Dr. Bohl makes the incision and frees up some muscle, ligaments, nerves, and vessels, the abnormal bone forming the coalition is visible. Using x-ray guidance, Dr. Bohl will remove the abnormal bone. He will then re-evaluate for normal hindfoot motion. Additional bone will be removed until radiographic and examination provide evidence of sufficient resection. The extensor digitorum brevis, a nearby muscle with minimal importance, is transferred into the defect where the coalition was previously to prevent inadvertant coalition regrowth. After this procedure, patients are in a splint for 2 weeks, but then come out of the splint and into early and aggressive physical therapy to maintain their gains in range of motion. Results are excellent, and many patients with coalitions of both ankles come back for the other side.
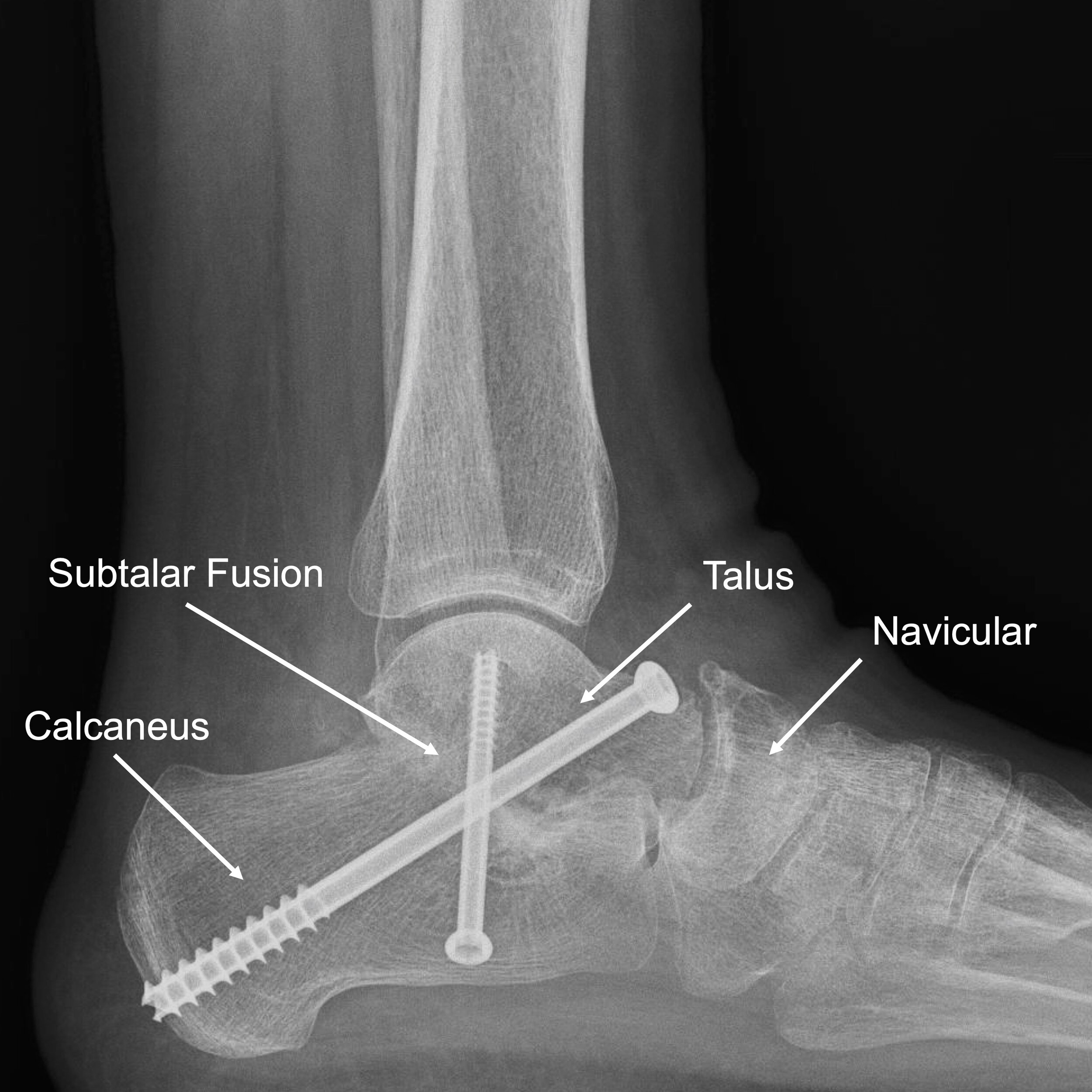
The second most common procedure that Dr. Bohl performs for tarsal coalitions is better for patients who are a little older, have developed arthritis of their hindfoot joints as a result of the coalition, and/or have a severe subtalar coalition. In such patients, simple resection of the coalition may result in a mobile, but painful, hindfoot. Hence, Dr. Bohl will resect the coalition, and then perform a fusion of the arthritic subtalar joint. While normal motion is not restored with this procedure, for selected patients, subtalar fusion may be the most reliable route to symptom relief. The postoperative recovery following subtalar fusion is a little more involved, including 2 weeks in a splint, 4 weeks in a cast, and then another 4 weeks in a boot. Dr. Bohl recommends a rolling knee scooter for patients undergoing this procedure.
Recurrence and Revision Surgical Treatment
Unfortunately, Dr. Bohl sees a fairly high volume of patients who have had failed tarsal coalition surgery at other hospitals. Tarsal coalitions are quite complicated, and surgeon experience with resection is critical. Dr. Bohl recommends patients have this procedure performed by an MD orthopaedic foot and ankle surgeon if at all possible.
When patients present having had prior tarsal coalition resection and persistent or recurrent symptoms, Dr. Bohl will typically recommend a fairly extensive imaging workup including both CT and MRI. The question becomes whether the problem is inadequate initial resection of the coalition, regrowth of the coalition, or development of arthritis following resection. It is critical that you bring your “operative report” from your prior procedure so that Dr. Bohl can understand what was done and what he can do to correct your problem.
Undergoing surgery once is hard enough, and undergoing revision surgery is an even bigger endeavor. Dr. Bohl will take as much time as you need to explain the circumstances and help you choose the best path to relief.